|
|
|
|
|
Case #2
|
Typical Clinical Presentation:
A 20-year-old male presented with a painless, hard subcutaneous mass in the popliteal fossa.
He stated that the mass had been present for several years and did not change in size.
-
Two words, "painless" and "non-growing" (or very slow growing), suggest that the lesion
described here is probably benign.
|
|
|
|
Characteristic Radiological Findings:
|
|
|

|
-
Plain radiograph demonstrated a pedunculated bony outgrowth at the proximal tibial metaphysis.
The lesion had a uniform, cartilagenous cap with stippled calcifications. The tibial cortex
and medulla were continuous with those of the lesion.
|
|
|
|
Pathological Findings:
|
|
|
|
The specimen consisted of a pedunculated lesion, 3 x 3 x 2cm, with a lobulated cartilage cap measuring up to 0.9cm in thickness.
|
|
|

|
-
Cross section through the lesion demonstrated mature trabecular and cortical bone with a uniform cartilage cap, less than 1cm in thickness. Few small islands of similarly appearing cartilage were present in the stalk and
at the resection margin.
|
|
|
|
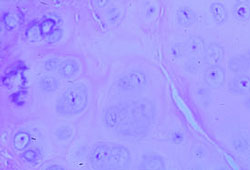
-
Higher magnification of a cartilage cap shows mature, focally calcified hyaline cartilage.
|
|
|
Diagnosis: Osteochondroma
|
|
Salient Points:
|
-
Most common skeletal sites include metadiaphyses of the femur and tibia at the knee (35%), proximal femur
and humerus, pelvis and scapula. This tumor does not occur in bones with membranous type of ossification.
-
Solitary osteochondromas may be either primary due to a developmental anomaly of bone, or secondary
following trauma. Unlike primary osteochondromas, secondary lesions are often seen in the phalanges
of the hands and feet and have their peak incidence in the 3rd and 4th decades of life. Multiple osteochondromas
represent an autosomal dominant hereditary disorder and are associated with bone deformities.
-
Clinical behavior. Osteochondromas are benign lesions with self-limited growth and are treated by simple excision.
Recurrence may develop when a portion of cartilage cap is left behind. That is why assessment of surgical margins is
important. Malignant transformation is more often seen in multiple hereditary osteochondromas.
Most common secondary malignancy is chondrosarcoma. The earliest pathologic sign of malignant transformation
to a low-grade chondrosarcoma is increased thickness of the cartilage cap.
The cap thickness will exceed 2cm and will show increased cellularity with mild to moderate cellular atypia.
- Experimental data:
There are many theories of osteochondroma pathogenesis. The older school of thought considers it a hamartoma arising from a portion of growth plate cartilage entrapped beneath the periosteum during skeletal growth. It is thought that the entrapped pieces continue to grow and ossify at the same rate as the adjacent bone. When skeletal maturity is reached, osteochondromas usually stop growing. Continued growth in skeletally mature individuals may signify malignant transformation. Molecular studies, however, suggest a neoplastic process for development and progression of osteochondroma. Clonal origin of of both sporadic and herediatry osteochondromas is supported by the discovery of the clonal cytogenetic abnormalities. These include deletions of regions q24 of chromosome 8 (EXT1 locus) and p11-12 of chromosome 11 (EXT2 locus) that lead to inactivation of EXT1 and EXT2 genes. Although the precise role of EXT genes remains unknown, they are thought to act as tumor supressors. It appears that the truly neoplastic part is the cartilagenous cap while the osseous part of the tumor is, probably, reactive. Bovee et al have shown loss of heterozygosity (LOH) and DNA aneuploidy in cells of the cartilagenous cap. It has been suggested that EXT inactivation is the initiating event in osteochondroma formation. Additional genetic alterations may be required for malignant transformation.
Available publications for the topic:
Osteochondroma
|
|
Selected References::
|
- Porter DE, Simpson AH. The neoplastic pathogenesis of solitary and multiple osteochondromas. J Pathol 1999;188:119-125
- Bridge JA, Nelson M, Orndal C, Bhatia P, Neff JR. Clonal karyotypic abnormalities of the hereditary multiple exostoses at chromosomal loci 8q24.1 (EXT1) and 11p11-12 (EXT2) in patients with sporadic and hereditary osteochondromas. Cancer 1998;82:1657-1663
- Bovee JVMG, Cleton-Jansen AM, Wuyts W, et al. EXT mutation analysis and loss of heterozygosity in sporadic and hereditary osteochondromas and secondary chondrosarcomas. Am J Hum Genet 1999;65:689-698
|
|
|



